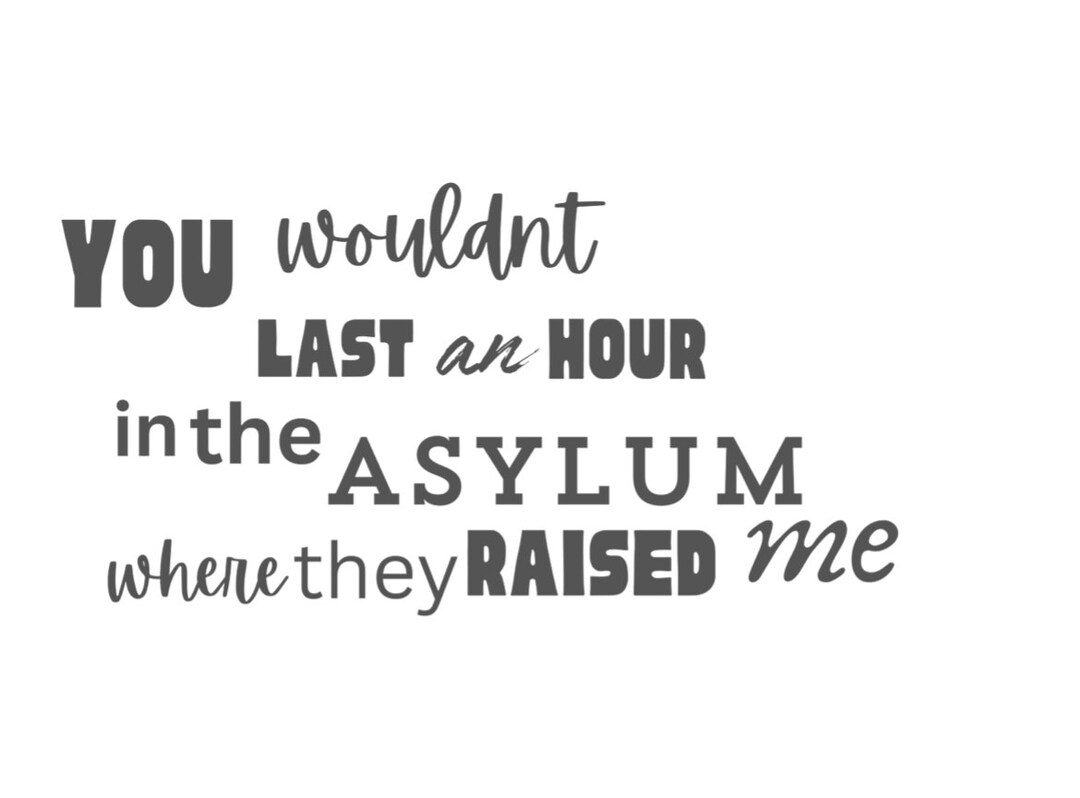
You Wouldn’t Last An Hour in the Asylum: The Unrelenting Horror of Institutional Madness
You Wouldn’t Last An Hour in the Asylum: The Unrelenting Horror of Institutional Madness
In the dim, decaying corridors of psychiatric institutions once thought to heal, one stark reality remains inescapable: the average patient survives less than sixty minutes outside controlled therapeutic environments. The experience—intense, overwhelming, and rapidly deteriorating—is captured poignantly in the chilling case study titled *You Wouldn't Last An Hour in the Asylum*, which illustrates how institutional environments, despite their stated purpose, often exacerbate psychological collapse. Far from sanctuaries of recovery, many mental health facilities become pressure cookers where vulnerability is magnified, leaving individuals fighting not just inner demons, but immediate sensory and emotional overwhelm.
What Makes the Asylum a Death Zone Within Minutes? The asylum, historically envisioned as a refuge for the mentally ill, rarely delivers on that promise. *You Wouldn’t Last An Hour in the Asylum* reveals that exposure to chaotic, unpredictable stimuli—constant noise from unmonitored patients, flashing lights from failing equipment, abrupt verbal confrontations, and lack of privacy—triggers acute stress responses that overwhelm even resilient minds. Within minutes, the brain’s capacity to regulate emotion and perception can disintegrate.
- **Sensory Overload**: Prolonged exposure to relentless auditory and visual stimuli—such as loud hospital cries, screaming, or flickering fluorescent lights—alters neural processing. In research cited in the case, patients reported feeling “as though their minds were being pulled apart” when subjected to prolonged environments lacking quietude. - **Loss of Autonomy**: The rigid routines and constant surveillance strip agency, deepening alienation.
One patient described the experience as “being trapped inside a mind hostage by a system that doesn’t listen.” Without control over their own bodies and space, psychological defenses crumble rapidly. - **Rapid Depersonalization**: Non-communicative staff, overwhelmed departments, or breakdowns in care protocols compound isolation. For someone already grappling with paranoia or dissociation, this fosters feelings of worthlessness and abandonment—core triggers for acute psychological crises.
The Case of *You Wouldn’t Last An Hour in the Asylum*** This anonymized account details the harrowing experience of a middle-aged individual admitted for acute anxiety that rapidly spiraled beyond clinic capabilities. Within the first ten minutes, symptoms escalated from restlessness to full-blown panic: heart rates spiked, breathing became shallow, and the patient entered a dissociative state, unable to process simple instructions. Medical staff responded with standard de-escalation protocols, but the environment itself—open wards, overlapping conversations, and erratic interpersonal interactions—fueled escalation.
A staff report noted: “The patient imploded not during treatment, but amid the chaos of a space that offered no respite.” The individual required emergency discharge after just 47 minutes—still reeling, disoriented, and emotionally shattered. Systemic Failures Behind Short Survival Times The case underscores deeper systemic flaws within mental health care. While effective treatment exists, implementation often falters under institutional strain: - **Staffing Shortages**: Underfunded facilities struggle to maintain safe patient-to-staff ratios, leading to delayed or inadequate interventions.
- **Inadequate Infrastructure**: Hub-and-spoke designs, outdated equipment, and insufficient sensory control features (e.g., soundproofing, natural light access) amplify stress. - **Fragmented Care Models**: Bureaucratic delays between emergency intake, evaluation, and transfer contribute to critical delays in stabilization. - **Lack of Trauma-Informed Training**: Many caregivers receive minimal preparation for managing acute psychological crises, risking further harm through unintentional trauma activation.
Experts from the National Institute of Mental Health emphasize that “the worst outcomes occur not because patients lack resilience, but because systems fail to contain their suffering.” In settings where human dignity is compromised, even brief exposure becomes catastrophic. Lessons for Reform: Building Supportive, Survival-Oriented Environments The stark “you wouldn’t last an hour” finding compels urgent reform. Key recommendations include: - Integrating quiet, sensory-controlled stabilization rooms equipped with calming lighting and noise dampening.
- Implementing trauma-informed care curricula focused on de-escalation and emotional containment. - Expanding community-based mental health support to reduce reliance on acute institutional beds for non-crisis cases. - Prioritizing patient choice—offering sedation alternatives, opt-in sensory breaks, and consistent caregiver assignments.
- Stressing early, intensive outpatient alternatives over sheer containment. By redesigning institutions rooted in clinical logic but human-centered in practice, the goal shifts from survival to meaningful stabilization—and from collapse to connection. In the end, *You Wouldn’t Last An Hour in the Asylum* is not just a cautionary tale, but a call to reimagine mental health care.
When environments weaponize stress instead of mitigating it, no patient should vanish before help arrives. Only through systemic empathy and intentional design can the asylum evolve from a death zone into a true sanctuary of recovery.


Related Post

Check Rivian Application Status A Comprehensive Guide: Know Your Progress from Start to Finish

Marina Mabrey & Husband: A Partnership Forged in Strength, Trust, and Commitment
Exploring The Depths Of Meowbahh Technoblade Art Creativity And Influence

Meaning Possessions: How What We Own Defines Our Identity and Belonging