Words to Scar Tissue: How Emotional Wounds Scar Deeper Than Games Ever Could
Words to Scar Tissue: How Emotional Wounds Scar Deeper Than Games Ever Could
Words to Scar Tissue explores the underrecognized reality that some emotional injuries run as deep and unyielding as the physical scars left by a surgical scar—especially when tied to trauma, loss, or betrayal. It’s a sobering look at how psychological wounds persist not just in memory, but in biology, behavior, and daily life. Where physical scars heal visibly, emotional and psychological scars often linger beneath the surface, shaping identity, relationships, and even physiological function.
Drawing from clinical psychology, neuroscience, and lived experience, this article unpacks the mechanisms of scarring, its lasting impacts, and pathways toward healing—revealing why trauma demands not just awareness, but deliberate, sustained care.
What Counts as a Scar Tissue Injury? Defining the Emotional Aftermath
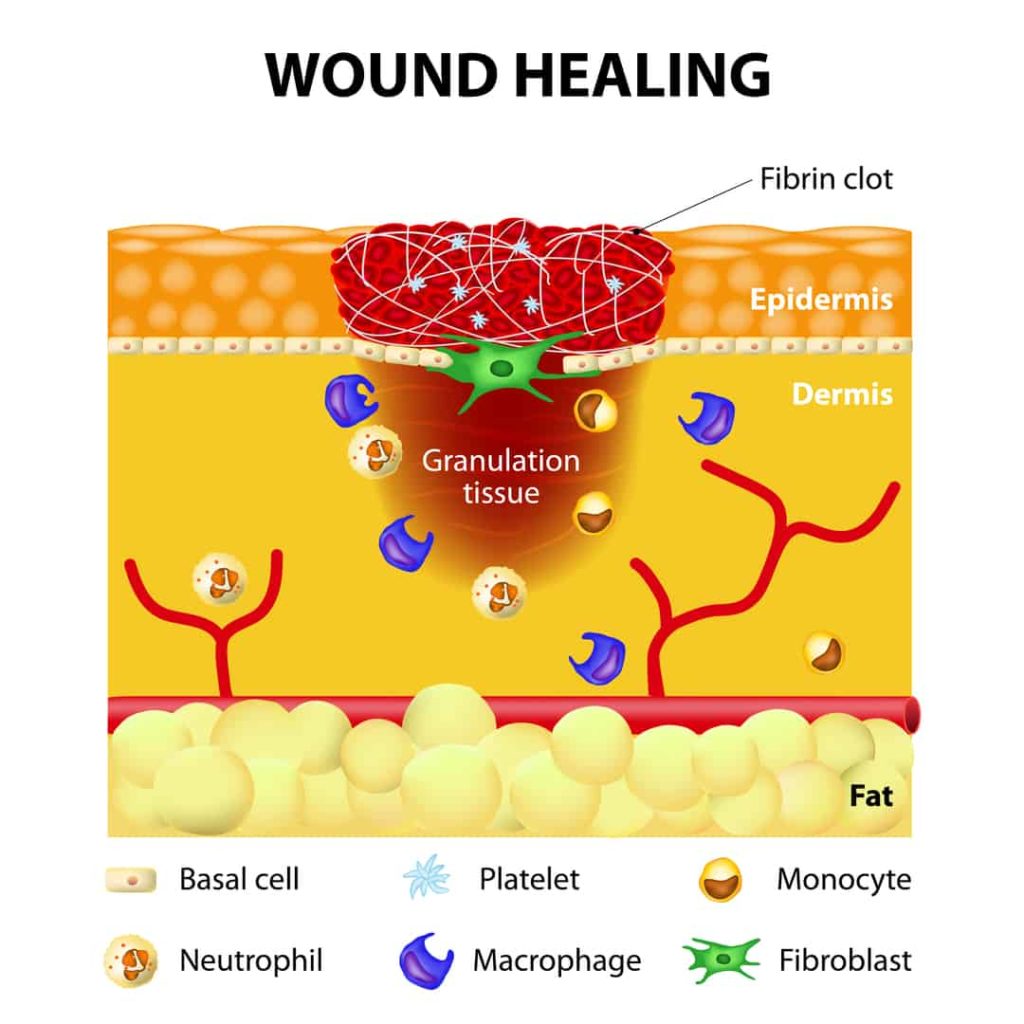
Emotional scar tissue forms when profoundly distressing events—such as childhood neglect, war, abuse, betrayal, or sudden loss—project lasting psychological damage.Unlike temporary stress, these wounds embed themselves through repeated emotional upheaval, chronic threat, or enforced helplessness. The brain’s stress response systems—particularly the hypothalamic-pituitary-adrenal (HPA) axis—react strongly to such experiences, altering neural pathways involved in emotion regulation, memory, and threat detection. The term “scar tissue” metaphorically emphasizes durability.
Just as scar tissue heals with limited elasticity, emotional scars reduce psychological flexibility. For instance, someone who experienced chronic childhood invalidation may develop a persistent fear of rejection, manifesting in anxiety during intimate relationships or avoidance of vulnerability. These patterns often strengthen over time, becoming invisible barriers to emotional safety and connection.
Researchers highlight that emotional scarring isn’t always immediate—some wounds lie dormant before activating under new stress, much like a scar tissue reaction delayed by infection. This delayed response complicates diagnosis and treatment, as symptoms like hypervigilance, emotional numbness, or chronic fatigue may be mistaken for personality traits rather than trauma sequelae.
Neurobiological Markers: The Physical Imprint of Psychological Injury
Modern neuroscience confirms that emotional scar tissue isn’t just metaphorical—it leaves tangible biological traces.Prolonged exposure to trauma elevates cortisol and adrenaline, disrupting brain regions like the amygdala, hippocampus, and prefrontal cortex. The amygdala, responsible for threat detection, becomes hyperactive, lowering the threshold for perceiving danger. Meanwhile, the hippocampus, critical for memory consolidation, may shrink—a physiological response linked to reduced emotional regulation and intrusive flashbacks.
* Studies using fMRI imaging reveal individuals with complex post-traumatic stress disorder (C-PTSD) display distinct neural activation patterns when recalling traumatic events, suggesting fiercely ingrained emotional circuitry. * Chronic stress also accelerates cellular aging via telomere shortening, connecting psychological scars directly to physiological decline. * The autonomic nervous system, responsible for fight-or-flight responses, remains chronically activated, contributing to conditions such as insomnia, chronic pain, and gastrointestinal disorders.
These changes illustrate why psychological wounds resist simple healing—because they rewire both mind and body.
Daily Life Under the Weight of Scar Tissue: From Behavior to Identity
The persistent nature of emotional scar tissue permeates nearly every dimension of functioning. Behaviorally, affected individuals may exhibit hypervigilance, emotional volatility, withdrawal, or compulsive avoidance.Relationships often suffer; trust erodes, emotional intimacy feels threatening, and boundaries become either rigid or porous. Cognitively, persistent rumination, self-criticism, and distorted self-perception—such as “I’m unworthy” or “I don’t deserve care”—tend to persist, reinforcing the cycle of distress. Emotionally, experiences of shame, grief, or emptiness may obscure the original cause, making recovery feel dim and unattainable.
Research on adverse childhood experiences (ACEs) confirms that individuals with high ACE scores face elevated risks not only for mental illness but also physical conditions like heart disease, diabetes, and autoimmune disorders. This convergence of psychological and physical suffering underscores the pervasive reach of emotional scar tissue. Examples of real-life impact are widespread: a previously successful executive struggling with managerial burnout that traces back to childhood bullying; a veteran managing PTSD symptoms years after service; a long-term caregiver battling chronic anxiety rooted in unresolved grief from a past loss.
Each carries a silent, internal injury—scar tissue woven into the fabric of daily existence.
Healing the Wound: Pathways Through Scar Tissue
Healing emotional scar tissue requires more than passive endurance—it demands intentional effort, understanding, and often, professional support. Evidence-based approaches emphasize safety, stabilization, and gradually reactivating emotional processing.Key elements include: - **Somatic therapies**, such as EMDR (Eye Movement Desensitization and Reprocessing) and sensorimotor psychotherapy, which address trauma stored in the body through controlled recall and grounded awareness. - **Cognitive-behavioral strategies**, helping individuals identify and reshape maladaptive thought patterns shaped by past injury. - **Mindfulness and regulation techniques**, fostering present-moment awareness to reduce hyperarousal and break cycles of rumination.
- **Narrative reconstruction**, allowing survivors to reclaim personal stories with compassion, challenging internalized shame. - **Social reconnection**, rebuilding trust through supportive relationships that counter isolation. Importantly, lasting change hinges on patience.
Unlike physical wounds, emotional scar tissue doesn’t heal overnight; small, consistent steps can gradually remodel neural pathways and restore psychological resilience. > “Healing isn’t erasing the scar—it’s learning to live beside it, not because you forget, but because you no longer fear its sting.” A growing cohort of mental health professionals stresses that suppression or denial only ossifies injury; openness, self-compassion, and structured therapy remain vital to dismantling psychological scarring.
The Broader Implication: Recognizing and Responding to Emotional Scar Tissue
Understanding scar tissue within emotional injury transforms public discourse and clinical practice.It shifts focus from blaming individuals for “weakness” to acknowledging injury as a legitimate, complex condition. Schools, workplaces, and healthcare systems increasingly adopt trauma-informed models—prioritizing safety, choice, and support to prevent repeated harm. On a societal level, recognizing scar tissue demands compassion.
When we see beyond surface behavior to the invisible wounds beneath, we foster environments where healing becomes not just possible, but probable. The metaphor of scar tissue reminds us that while scars are indelible, they are not unbreakable—understanding their depth can guide us toward more humane, effective care. In the end, Words to Scar Tissue reveal a stark truth: emotional pain etches itself deeply, but it does not define forever.
With recognition, compassion, and evidence-based care, the invisible wounds may heal—and in doing so, transform lives beyond recovery.


Related Post

Taylor Swift’s Musical Odyssey: All Albums in Order, Chronologically and in Impact
Cambia Play Store a Español: El Proceedings Clave para Usuarios de Todo el Mundo

How the Perfect Crack in Hybrid Pastry Reveals Secrets Experts Hiden in 2013 Crossword Clues

Unblocked Pong: The Timeless Arcade Classic That Defies Restrictions

