The Power of Precision: How Data-Driven Public Health Strategies Are Transforming Global Wellbeing
The Power of Precision: How Data-Driven Public Health Strategies Are Transforming Global Wellbeing
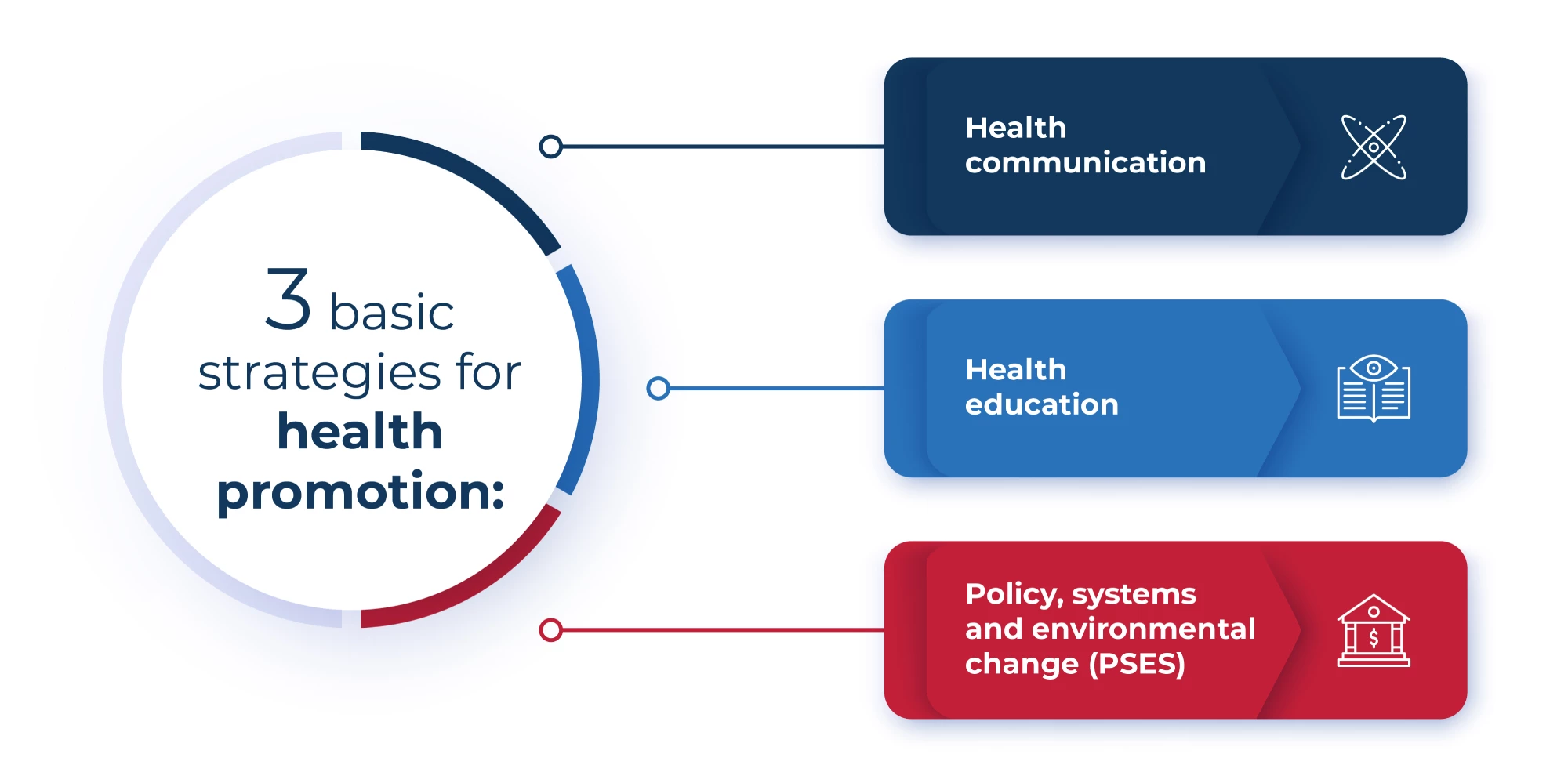
In an era where infectious outbreaks, chronic disease burdens, and lifestyle-related health risks evolve at unprecedented speed, precision public health has emerged as a game-changing approach. Defined by the strategic integration of real-time data, advanced analytics, and targeted interventions, precision public health moves beyond one-size-fits-all models to deliver interventions calibrated to the needs of specific populations. This shift reflects a growing recognition that effective health outcomes depend not just on broad policies, but on understanding the nuanced patterns shaping local and global populations.
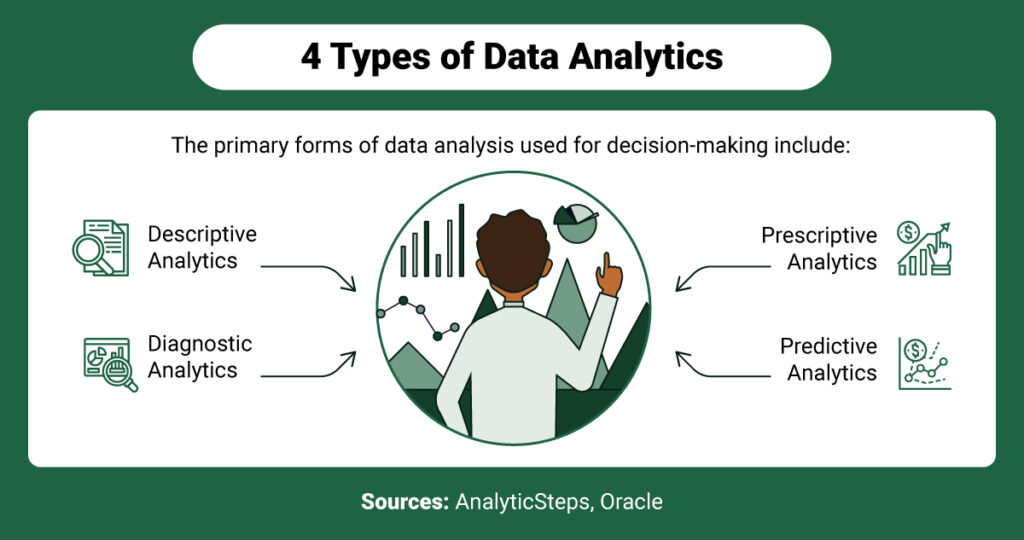
At the core of precision public health is the transformation of data into actionable insight. Durable health gains now hinge on the ability to collect, analyze, and act on diverse datasets — from genomic sequencing of pathogens to socioeconomic indicators and behavioral trends. “Precision means moving away from ‘non-specific’ approaches and toward tailored solutions,” explains Dr.
Maya Thompson, an epidemiologist at the Global Health Institute. “By identifying who is at highest risk, when and where outbreaks emerge, and why certain groups respond better to interventions, we can allocate resources with surgical accuracy.”
Harnessing Big Data and Real-Time Surveillance
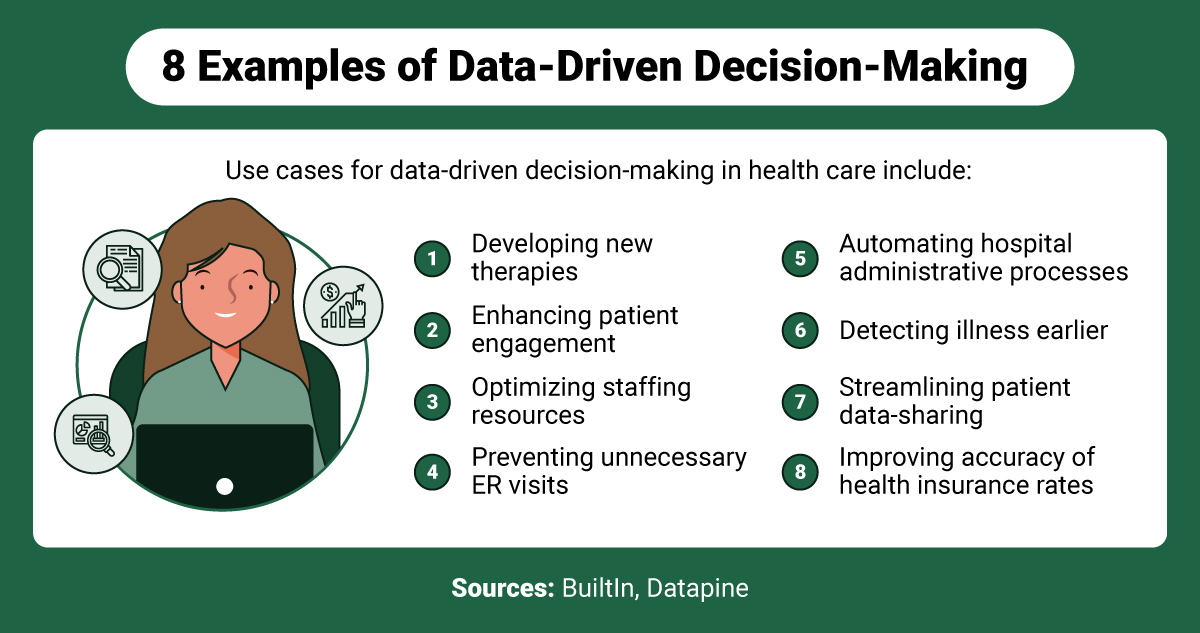
Modern epidemiology no longer relies solely on traditional reporting methods. Instead, public health authorities leverage digital surveillance systems powered by artificial intelligence and machine learning to detect early warning signals.For instance, syndromic surveillance platforms aggregate anonymized data from emergency department visits, pharmacy sales, and even mobile health applications to spot anomalies that may indicate disease spread. During the recent monkeypox outbreak, such systems enabled countries to identify cases within hours of symptom presentation, dramatically shortening response times. This real-time intelligence supports rapid deployment of targeted measures.
Instead of broad lockdowns or nationwide vaccination campaigns, authorities can focus efforts on high-risk neighborhoods, high-transmission settings, or vulnerable demographic clusters. For example, during measles outbreaks in urban centers, data analysis revealed clusters tied to specific schools or communities with low vaccination rates, allowing clinics to organize focused immunization drives that achieved over 90% coverage in key cohorts. < Jimmy highlights a critical enabler: predictive modeling.
Using historical and current data, models now forecast disease trajectories with increasing reliability. These models account for variables such as climate patterns, population density, mobility trends, and prior intervention outcomes. Such forecasting empowers decision-makers to pre-position medical supplies, staff, and public messaging before crises escalate.
Equity and Community-Centric Design in Precision Approaches
While technological sophistication advances, precision public health emphasizes equity. Early implementations risked widening disparities if data collection excluded marginalized groups or if interventions focused only on dominant demographics. Today, leading programs prioritize inclusive data frameworks that capture socioeconomic, cultural, and geographic diversity.Community engagement remains central. Local stakeholders — from grassroots organizations to faith leaders — help interpret data through cultural lenses, ensuring interventions resonate and gain trust. In rural sub-Saharan Africa, mobile-based health platforms paired with community health workers have improved maternal and child health outcomes by up to 35% in underserved regions.
By blending local knowledge with algorithmic insights, public health initiatives become both data-informed and person-centered.
Success Stories Across the Globe
- In South Korea, integration of national health records with mobile contact tracing transformed the COVID-19 response. By rapidly identifying and isolating transmission chains, the country avoided prolonged restrictive measures, maintaining economic stability while keeping case rates manageable even during surges.- In Brazil, predictive analytics targeting high-risk urban favelas dramatically reduced dengue fever incidence by enabling targeted vector control and public awareness campaigns before outbreaks peaked. - During the 2022 polio surge in Afghanistan and Pakistan, precision mapping of at-risk children via census and community surveys enabled vaccination campaigns to reach 98% of target populations in hard-to-access areas. These cases underscore how precision public health not only enhances response efficacy but also strengthens resilience against future threats by building adaptive, evidence-based systems.
The Future: Scaling Precision with Ethical Innovation The momentum behind precision public health continues to grow, driven by advances in genomics, wearable technology, and AI interoperability. Yet, scaling these approaches requires careful attention to data privacy, algorithmic fairness, and global collaboration. Experts stress that transparency in data use, community consent frameworks, and safeguarding against bias in predictive models are not optional—they are essential to maintaining public trust.
Furthermore, interoperability across health information systems remains a critical challenge. Fragmented data silos can hinder timely insights, especially in low-resource settings. International partnerships and investments in digital infrastructure are vital to ensure that precision tools benefit all populations equitably.
Looking ahead, precision public health is evolving from a niche strategy into a foundational pillar of global health policy. Its success depends not only on technological innovation but on inclusive design, ethical governance, and sustained investment. As nations confront an increasingly interconnected and dynamic health landscape, precision remains the most reliable compass for safeguarding population wellbeing — proving that the future of health is not just data-driven, but deeply human.
Ultimately, precision public health stands as a testament to what collective action, powered by insight and empathy, can achieve. By turning vast streams of information into lifelines for communities, it redefines what is possible when science meets equity.