The Age of Modern Medical Science: Unraveling the Revolution That Transformed Human Health
The Age of Modern Medical Science: Unraveling the Revolution That Transformed Human Health
From ancient herbal remedies to AI-driven diagnostics, modern medical science has undergone a seismic transformation—reshaping how diseases are understood, treated, and, in many cases, cured. What began as fragmented knowledge rooted in tradition has evolved into a data-rich, technology-powered discipline where breakthroughs emerge at an accelerating pace. This historical overview traces the pivotal developments that define the age of modern medicine, highlighting key milestones, visionary figures, and the enduring impact of human ingenuity on global health.
The Birth of Scientific Medicine The foundation of modern medical science rests on the shift from mystical and superficial healing practices to evidence-based inquiry. In the 19th century, the germ theory of disease, championed by Louis Pasteur, dismantled long-held miasma theories and redefined contagion. Pasteur’s work proved that microorganisms—bacteria and viruses—were the root cause of many illnesses, a revelation that set medicine on a path toward precision.
As historian Joyce Appleby notes, “This was medicine’s awakening: symptoms ceased to be the sole focus, and pathogens became targets.” Concurrently, Robert Koch’s postulates provided a systematic way to link microbes to specific diseases, enabling targeted treatments. This scientific rigor marked medicine’s definitive break from superstition and laid the groundwork for microbiology. Statistical rigor and public health emerged as powerful allies in the fight against disease.
Pioneers such as John Snow, who mapped cholera outbreaks in 1854 London, demonstrated the power of data visualization in epidemiology, charting the deadly link between water contaminated with *Vibrio cholerae* and the city’s Broad Street pump. His work underscored the principle that population health could be systematically studied and improved. Decades later, Florence Nightingale transformed healthcare logistics through meticulous data collection, proving conclusively that sanitation reduced mortality far more than medical interventions alone.
Her legacy underscored a truth still central today: hospital design, hygiene protocols, and preventive care are as vital as treatment. The Rise of Surgical Innovation Advances in surgical practice redefined the limits of human intervention. Joseph Lister’s introduction of antiseptic techniques in the 1860s drastically reduced post-operative infections, turning surgery from a high-risk gamble into a reusable tool for saving lives.
By applying carbolic acid to instruments and wounds, Lister reduced mortality rates in amputations by over 70%, establishing sterility as standard practice. This breakthrough unlocked new frontiers—from organ transplants to minimally invasive techniques—validating surgery as a cornerstone of modern medicine. The 20th century ushered in revolutionary pharmacological discoveries.
The discovery of penicillin by Alexander Fleming in 1928 and its subsequent development into a usable drug by Howard Florey and Ernst Chain in the early 1940s revolutionized infection treatment. For the first time, previously fatal bacterial infections—such as pneumonia and sepsis—became curable. This antibiotic era laid the foundation for treating not just individuals but entire public health crises, transforming medicine into a preventive and curative force.
Vaccines emerged as medical triumphs born of both science and compassion. Edward Jenner’s smallpox vaccine in 1796 initiated a lineage culminating in Jonas Salk’s inactivated polio vaccine in 1955 and Albert Sabin’s oral version in the 1960s. These innovations drove polio to near extinction, a disease once feared across continents.
Today, mRNA vaccines built on decades of research—including work on mRNA platforms pioneered by scientists like Katalin Karikó—delivered in under a year during the COVID-19 pandemic, showcasing medicine’s capacity to leapfrog. Imaging technology redefined diagnostics. Wilhelm Conrad Röntgen’s discovery of X-rays in 1895 opened a window into the human body invisible to earlier tools.
Decades later, Godfrey Hounsfield and Allan Cormack’s development of computed tomography (CT) in the 1970s enabled 3D cross-sectional viewing, revolutionizing internal diagnosis. Magnetic resonance imaging (MRI), introduced in the 1980s, offered unprecedented soft-tissue detail without radiation, improving detection of brain disorders, cancers, and musculoskeletal conditions. These tools not only enhanced accuracy but empowered earlier interventions, shifting medicine toward prevention.
Biotechnology and genomics have unlocked the blueprint of life itself. The completion of the Human Genome Project in 2003 marked a genomic watershed, decoding over 20,000 genes and enabling personalized medicine. Pharmacogenomics now tailors drug regimens to individual genetic profiles, minimizing side effects and boosting efficacy.
CRISPR-Cas9 gene editing, developed in the 2010s, offers the power to correct genetic defects—raising both hope and ethical questions about the future. “We’ve moved from reading the genetic code to rewriting it,” observes geneticist Jennifer Doudna, highlighting medicine’s newfound agency. Digital health and artificial intelligence now extend medicine into real time and predictive analytics.
Wearable devices track heart rates, glucose levels, and sleep patterns, generating continuous health data. Machine learning algorithms parse millions of medical records, identifying patterns invisible to clinicians—enabling early disease detection, drug discovery, and real-time public health monitoring. AI-driven tools now assist radiologists in spotting anomalies, reduce diagnostic errors, and accelerate clinical trials.
These innovations signal medicine’s next evolution: a seamless, data-driven ecosystem where care anticipates needs before illness strikes. Public health infrastructure strengthened by modern medical science has drastically reduced global mortality. Life expectancy rose from around 40 years in 1900 to over 73 years by 2020, driven by vaccinations, improved maternal care, sanitation, and disease surveillance.
Yet challenges persist—antibiotic resistance, emerging zoonotic diseases, and health inequities—requiring ongoing vigilance and global cooperation. At its core, the age of modern medical science is defined by an unrelenting pursuit of understanding and healing. Each breakthrough builds on prior knowledge, weaving a complex tapestry that continues to expand.
From lab benches to nationwide health systems, medicine’s transformation is not just historical—it is alive, evolving, and saving lives across every corner of the world.
The Pillars of Scientific Method in Medical Advancement
A defining feature of modern medical science is its unwavering commitment to empirical rigor. The scientific method—hypothesis, experimentation, validation—has become the bedrock of innovation, ensuring treatments are not based on tradition but on measurable evidence.This disciplined approach began with figures like Pasteur and Koch, who relied on controlled observation and reproducible results to validate germ theory. Today, clinical trials with rigorous statistical analysis, peer review, and regulatory oversight ensure new therapies are both safe and effective before reaching patients. “Science doesn’t just describe disease—it tests solutions,” asserts bioethicist Arthur Caplan, emphasizing how methodical inquiry turns discovery into reliable care.
Epidemiology and the Science of Prevention
While treatment has advanced dramatically, prevention through epidemiology has reshaped global health outcomes. Cities like London in the 1850s saw cholera outbreaks decimated when John Snow mapped infections and eradicated the Broad Street pump source—proof that data-driven intervention saves lives. Decades later, Florence Nightingale’s sanitation reforms cut hospital mortality, underscoring that statistics and systemic change drive prevention.Today, epidemiologists use vast datasets—from surveillance systems to AI models—to track disease spread, forecast outbreaks, and design public health strategies. During the COVID-19 pandemic, real-time modeling guided lockdowns, vaccine rollouts, and resource allocation, illustrating epidemiology’s power in safeguarding populations. This proactive discipline reveals medicine’s dual mission: heal the sick and shield the many.
The Shift from Reactive to Proactive Care
Modern medical science has moved from a reactive model—treating symptoms after onset—to proactive prevention and early detection. Innovations in imaging, genomics, and biomarkers now identify diseases like cancer and cardiovascular disorders in pre-symptomatic stages. For example, low-dose CT screening detects lung cancer years before noticeable symptoms, improving cure rates by 20% or more.Similarly, genetic testing for BRCA mutations enables at-risk individuals to take preventive action—whether enhanced screening or prophylactic surgery. Wearables continuously monitor vital signs, alerting users to irregular heart rhythms or glucose spikes that may precede crises. This paradigm shift—empowering individuals and clinicians with foresight—marks a transformative era where medicine anticipates, intervenes early, and helps millions avoid preventable suffering.
Ethics, Equity, and the Future of Medical Innovation
With great power comes great responsibility. The rapid pace of medical innovation has sparked urgent ethical debates around access, consent, and genetic modification. Gene-editing tools like CRISPR raise profound questions: When is it acceptable to alter human DNA?How do we prevent inequitable distribution of cutting-edge therapies? History warns: without ethical guardrails, progress risks widening health disparities. Yet these challenges also fuel inclusive dialogue—between scientists, policymakers, and communities—aimed at inclusive and responsible innovation.
“We are not just building better treatments—we’re shaping the moral framework of healthcare for generations,” reflects Dr. Paul Farmer, co-founder of Partners In Health, reminding us that medicine’s legacy is defined not only by science but by justice. Through every era, modern medical science has evolved from observation to intervention, from treatment to prevention, and from isolation to integration.
What began with a single microscope’s lens has become a global network of knowledge, technology, and compassion—a journey that continues to redefine human health, one breakthrough at a time.




Related Post
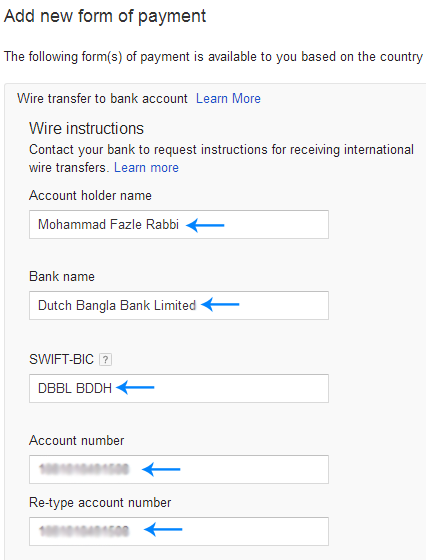
Update Your Gooogle AdSense Bank Details in Minutes—Simplified Process Promise

Dell Dimension: The Powerful Workstation Redefining Productivity at Every Desk

Stanford Rn New Grad Program Hired Part 4: Mastering Health Care Advancement Through Strategy and Insight

West Papua Unraveling: The Rising Flame of the Free Papua Movement

