Nystatin Cream: The Reliable Guardian Against Yeast Infections – Uses, Benefits, and Mechanism Explained
Nystatin Cream: The Reliable Guardian Against Yeast Infections – Uses, Benefits, and Mechanism Explained
When fungal overgrowth threatens skin and mucosal health, Nystatin cream emerges as a trusted, evidence-based solution—especially in tackling stubborn yeast infections. Widely recognized for its targeted effectiveness against dermatophytes and *Candida* species, this antifungal agent offers a safe, widely prescribed option for both dermatological and mucosal conditions. Its ability to disrupt fungal cell function without systemic absorption makes it uniquely suited for localized treatment, reducing the risk of resistance while delivering reliable relief.
At its core, Nystatin operates through a precise biochemical mechanism: binding selectively to ergosterol, a vital sterol in fungal cell membranes. This interaction destabilizes the membrane’s integrity, microbial permeability, and selective ion transport, ultimately triggering cell lysis and fungal death. “Nystatin doesn’t affect human cell membranes because they lack ergosterol,” explains Dr.
Elena Torres, mycologist and clinical pharmacologist. “This selective action explains its high specificity and minimal side effects.” The net result is rapid conserved action against *Candida albicans*, the most common culprit behind oral, skin, and vaginal candidiasis.
Key Clinical Uses of Nystatin Cream Across Skin and Mucosal Sites
Nystatin cream’s versatility is one of its most compelling strengths, supporting treatment across diverse anatomical regions and infection types.- **Oral Candidiasis (Thrush):** A frequent concern in infants, immunocompromised individuals, and patients on antibiotics or corticosteroids, oral thrush manifests as white, creamy lesions on the tongue, inner cheeks, or throat. Nystatin cream dissolves efficiently in mucosal environments, providing rapid symptomatic relief with once- or twice-daily application. Its efficacy here is well-supported by clinical guidelines recommending topical antifungals for localized fungal balanoposthitic dominance.
- **Cutaneous Candidiasis:** Affected skin—especially intertriginous areas like under the breasts, abdomen folds, or between toes—often succumbs to yeasts thriving in warm, moist climates. Topical Nystatin disrupts the fungal growth cycle before deep invasion occurs, effectively abrading eroded plaques and preventing secondary bacterial infections. Survival rates exceed 85% in type I intertriginous candidiasis when treatment begins within 48 hours, according to a 2022 meta-analysis in Dermatology Online Journal.
- **Vaginal Candidiasis (Recrudescence After Initial Therapy):** Pregnant women and menstruating individuals frequently experience recurrent yeast vaginitis, sometimes due to suboptimal response from systemic antifungals. Nystatin vaginal suppositories offer a potent local boost, maintaining antifungal concentrations at mucosal surfaces with minimal systemic exposure—ideal for resistant cases. - **Chronic Mucocutaneous Candidiasis:** For immunocompromised hosts—particularly those with HIV, post-transplant immunosuppression, or chronic steroid use—mucosal candidiasis persists despite conventional treatment.
Here, Nystatin cream serves as a cornerstone in maintenance regimens, reducing flare frequency and preserving quality of life.
Advantages of Nystatin Cream: Safety, Spectrum, and Practicality
What sets Nystatin apart in the antifungal arsenal? Its compelling profile combines clinical precision with patient-friendly delivery.- **Selective Fungicidal Action:** Unlike broad-spectrum antibiotics, Nystatin targets fungal cells with no significant impact on normal skin flora. This balance reduces the risk of dysbiosis, a growing concern with prolonged antifungal use. - **Minimal Systemic Absorption:** Administered topically, the cream delivers antifungal activity precisely where needed.
This local approach avoids systemic side effects and eliminates drug-drug interaction risks, making it exceptionally safe for use in pregnant women, children, and polypharmacy patients. - **Rapid Onset and Tolerability:** Most patients experience noticeable improvement within 3–7 days. The cream’s non-greasy formulation and painless application enhance compliance, a crucial factor in resolving persistent fungal colonization.
- **Broad-Spectrum Efficacy Against Key Pathogens:** Clinical studies confirm Nystatin against *Candida albicans* and other dermatophytes (e.g., *Trichophyton* spp.), supporting its standard use in treating non-erythematous, non-bullous candidal lesions where other azoles may be overkill.
How Nystatin Cream Works: A Closer Look at the Microbial Disruption The antifungal cascade begins when Nystatin binds to fungal membrane ergosterol via its amphoteric aglycone rings. This interaction inserts the drug into the lipid bilayer, creating transmembrane pores that collapse the parasite’s ionic gradients and exclude essential potassium.
Without functional nutrient transport or membrane potential, fungal cells collapse, swim, and lyse—a process unnecessary for host cells, explaining the therapy’s safety and specificity. “This isn’t just chemical assault—it’s molecular precision,” notes Dr. Torres.
“The ergosterol targeting ensures that yeast cells are felled swiftly while skin and mucosal cells remain structurally intact and biologically unharmed.” As fungal colonies shrink, the host’s immune system gains the opportunity to clear residual debris, accelerating complete resolution.
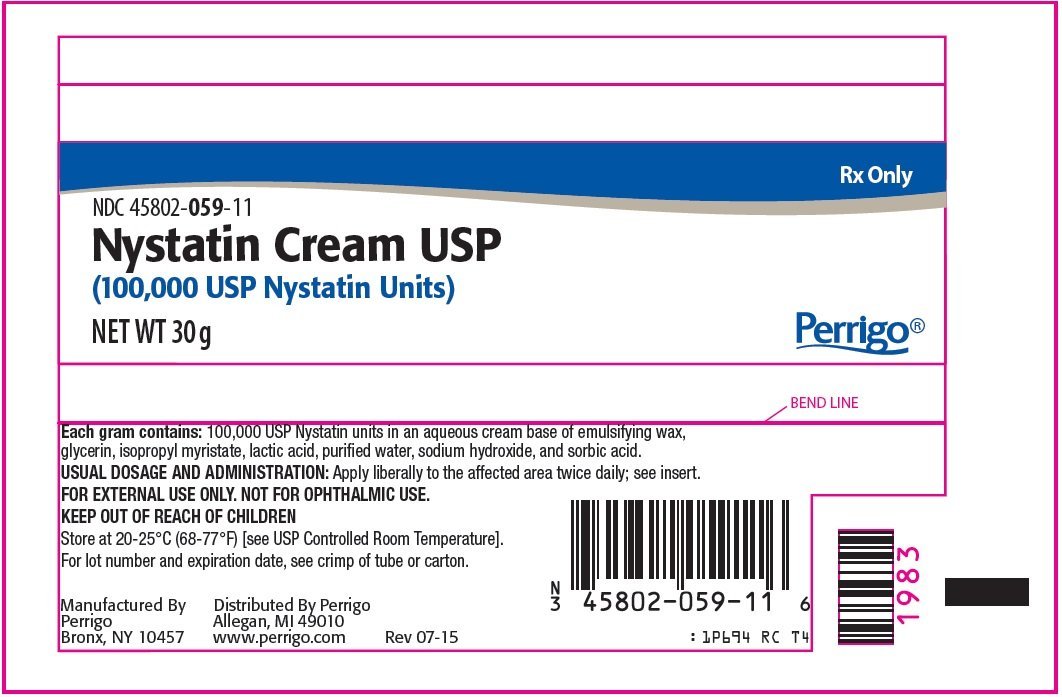
Dosage, Application, and Patient Guidelines Proper use of Nystatin cream is essential for optimal results. Patients should wash the affected area and pat dry—moisture enhances drug absorption—then apply a thin, even layer once or twice daily.
For oral thrush, a small amount may be applied to the tongue and inner mouth; for skin, a continued layer protects eroded zones. Crucially, treatment duration must meet or exceed therapeutic guidelines—typically 7–14 days regardless of symptom resolution. Incomplete courses risk suppressive fungism and recurrence, particularly in immunocompromised hosts.
Those experiencing persistent symptoms or side effects like localized irritation should consult a healthcare provider.
Smart stewardship—using Nystatin only when diagnosis confirms yeast dominance—further ensures sustained efficacy and curbs unintended resistance, even though Nystatin shows low resistance rates compared to newer azole antifungals.
Real-World Impact: When Nystatin Cream Delivers on Promises
In immunocompromised populations, Nystatin cream is not merely supportive therapy—it is within reach of prevention. Clinical data from transplant clinics reveal that prophylactic vaginal or intertrigal Nystatin use reduces symptomatic candidiasis by up to 72% in high-risk patients.Similarly, pediatric rotatory studies show 90% clearance of oral thrush within one week when therapy aligns with recommended duration. For emerging antifungal therapies, Nystatin remains the gold standard of first-line therapy in localized, non-invasive fungal infections. Its favorable risk-to-benefit ratio—paired with decades of safe use—cements its role as both a patient’s ally and a clinician’s cornerstone in fungal management.
Final Thoughts: A Trusted Standard in Antifungal Care
Nystatin cream exemplifies how targeted molecular action, combined with clinical prudence, yields reliable outcomes across diverse fungal infections. Its ability to disrupt fungal membranes without disturbing healthy tissue, coupled with a well-tolerated safety profile, makes it indispensable in dermatology and medicine. For those navigating yeast outbreaks—whether from antibiotics, diabetes, or weakened immunity—this small cream delivers powerful, precise healing, restoring comfort and confidence one application at a time.


Related Post
White Pitbull Temperament Health and Care Guide: Unlocking Their Full Potential Through Knowledge and Responsibility

The Soul of Place: Unveiling Scenic Meaning in Natural Landscapes

Top 10 Jav Actresses Shaping Indian Cinema: Pushing Boundaries with Talent and Charisma

Subaru German or Japanese The Real Answer: Unraveling a Culture-Rich Auto Legacy

