Netherlands Healthcare: A Global Benchmark in Quality, Access, and Innovation
Netherlands Healthcare: A Global Benchmark in Quality, Access, and Innovation
At first glance, the Dutch healthcare system appears like a finely tuned machine—seamless, adaptive, and remarkably effective. Ranked among the top-performing healthcare systems worldwide, the Netherlands delivers high-quality care with remarkable access, combining universal coverage, patient autonomy, and continuous innovation. Unlike many national systems that struggle between equity and efficiency, the Netherlands has carved a unique path that prioritizes both medical excellence and individual responsibility, resulting in outstanding health outcomes and high public satisfaction.
What sets this model apart is not just universal coverage, but a carefully balanced architecture built on accessibility, competition, and preventive care.
Central to the Netherlands’ success is its dual structure of public and private provision, operating under a mandatory health insurance mandate. All residents must enroll in a regulated sickness fund—either public or private—funded through a mix of payroll contributions and income-based premiums, with significant government subsidies ensuring affordability.
This system ensures universal access without creating barriers based on income or pre-existing conditions. Patients enjoy broad choice among providers, and medical professionals operate in an environment that encourages choice and accountability, rather than bureaucratic rigidness. As Dr.
Elise van Dijk, a public health expert at Leiden University, notes: “The Dutch model mirrors a delicate harmony—where citizens are trusted consumers, providers compete transparently, and preventive care is actively incentivized.”
Quality of Care: Rigor Built on Transparency and Evidence
The Netherlands consistently ranks among the top ten nations in global healthcare assessments, including the OECD Health Statistics and the World Health Organization’s World Health Report. A defining strength is the emphasis on evidence-based medicine and continuous quality improvement. Hospitals and clinics participate in national benchmarking systems that track performance on key indicators—from vaccination rates to emergency response times—ensuring accountability and consistency across regions.- **National Benchmarking:** Public and private providers are ranked annually on clinical outcomes, patient safety, and satisfaction. This data-driven approach drives innovation and performance across the board. - **Shared Decision-Making:** General practitioners play a pivotal role, acting as gatekeepers and coordinators who guide patients toward appropriate specialist or hospital care using real-time data and patient preferences.
- **High Preventive Standards:** Routine screenings, private health checkups, and public awareness campaigns underpin early detection. The Netherlands leads Europe in cancer screening uptake, with over 90% of eligible citizens undergoing定期 mammograms and colonoscopies. These systems collectively ensure high-quality, reliable care.
With life expectancy exceeding 82 years and low maternal and infant mortality rates, the system proves effective not just in treatment, but in sustaining long-term population health.
Accessibility: Universal Coverage with Unique Flexibility
Accessibility lies at the core of the Dutch healthcare philosophy. Every citizen and legal resident has guaranteed access to essential medical services without upfront cost at the point of care—deductible premiums and co-payments exist but do not restrict essential treatment.Wait times for specialist appointments and surgeries remain constrained through robust capacity planning and regional distribution of services. - **Geographic Equity:** Despite dense urban centers and rural regions, Dutch residents face minimal disparities in healthcare availability. Satellite clinics and telemedicine extend coverage to remote areas, supported by digital health platforms.
- **Affordable Access:** While annual fees apply, they are income-adjusted and capped, shielding low-income individuals from financial hardship. The government mandates transparency in pricing and service bundling through the ZIN (Zorgindeling Nederland), reducing surprise billing. - **Telemedicine and Digital Inclusion:** A national digital health infrastructure—including secure patient portals and electronic medical records—enhances continuity of care, especially for chronic disease management.
During the pandemic, telehealth usage surged, proving adaptable even under pressure. Patients report high satisfaction with continuity of care, timely referrals, and respectful consultation practices. Despite occasional bottlenecks in non-urgent services, the system delivers broad, reliable access—an issue often cited as a cornerstone of Dutch satisfaction.
What Makes the Netherlands Healthcare Model Exceptional
Beyond quality and access, the Netherlands’ greatest strength lies in its integration of prevention, transparency, and patient empowerment. The system rewards proactive health management through structured wellness programs, employer incentives for healthy workplaces, and public campaigns that normalize lifestyle interventions. Unlike many systems where preventive care is underfunded or stigmatized, the Dutch model treats prevention as a public good, seamlessly woven into daily life.- **Strong Institutional Trust:** High trust in care providers—backed by a reputation for personalized, responsive service—fuels compliance and engagement. - **Competition with Accountability:** Private insurers and clinics compete fiercely on quality and speed, maintaining innovation without sacrificing equity. - **Data-Driven Governance:** Real-time health data analytics inform policy, enabling agile responses to emerging challenges like pandemics and chronic illness trends.
This synergy of systems—regulated yet dynamic, public yet participatory—creates a healthcare ecosystem that is both resilient and responsive.
As the Dutch model continues to evolve, it offers a compelling blueprint for nations seeking to balance universal coverage with excellence. It proves that high-quality, accessible healthcare is achievable not through single-payer rigidities or unregulated privatization, but through thoughtful integration, open competition, and unwavering public commitment.
With clear metrics, patient-centered design, and continuous improvement at its core, Netherlands healthcare does more than treat illness—it builds healthier societies, one informed choice and skilled professional at a time.




Related Post
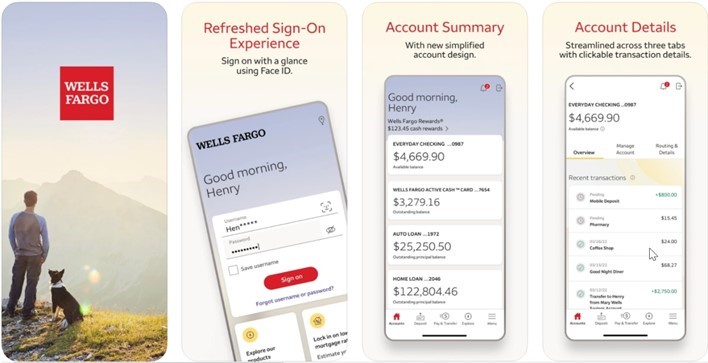
Wells Fargo App Login: Your Key to Effortless, Secure Account Access

Big Brother VIP Albania 4: Your Ultimate Guide to 24/7 Live Access and Behind-the-Scenes Intimacy

Master Apple ID Login: The Essential Guide to Secure, Seamless Access

Nissan Financial Login Access Your Account Easily — No More Hassle, Just Seamless Control

