Channel On Fox News Unpacks the Surge in U.S. Mental Health Crises
Channel On Fox News Unpacks the Surge in U.S. Mental Health Crises
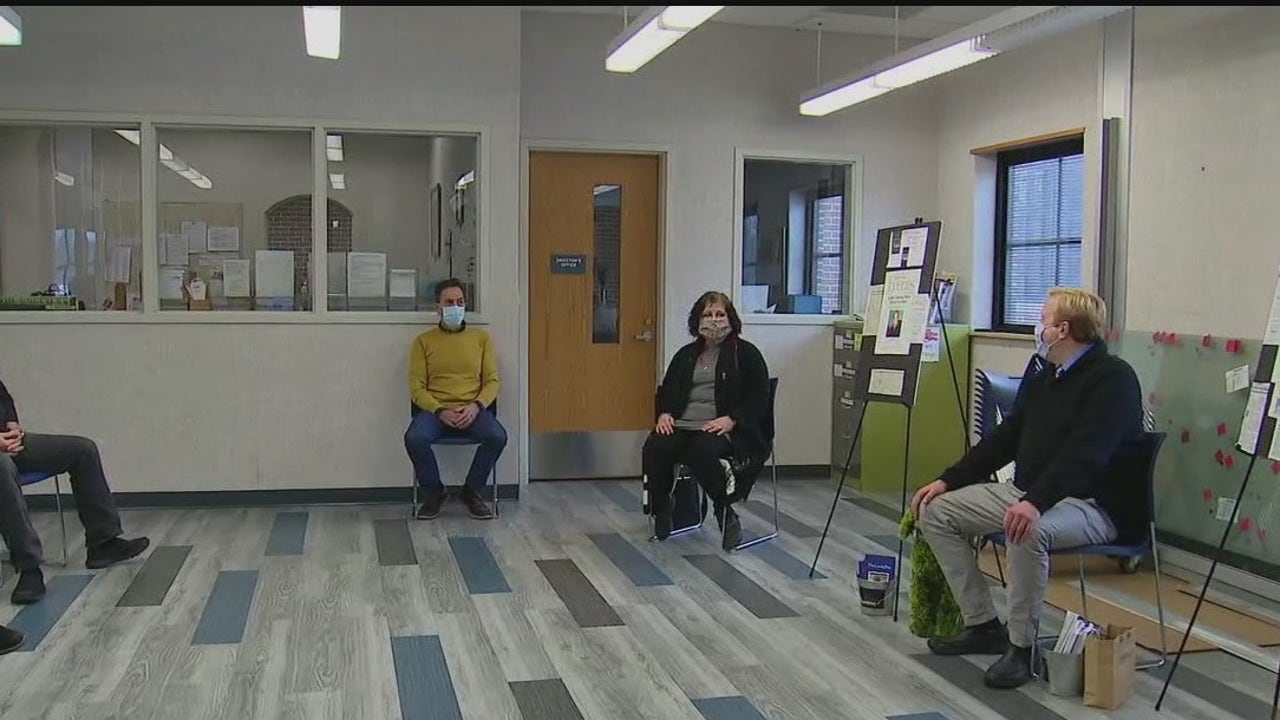
As mental health challenges intensify across the United States, Sandra On Fox News delivers a hard-hitting examination of the alarming rise in anxiety, depression, and substance use—driven by pandemic trauma, economic strain, and a stark shortage of care access. Local and national data reveal that over 40% of Americans now report persistent feelings of hopelessness, a significant spike from pre-pandemic levels. With experts warning of a looming crisis, public discourse is shifting toward urgent calls for reform in mental health policy, funding, and community support.
From Crisis Spikes to Systemic Shortcomings: The Data
Nationwide, mental health diagnoses have surged across all age groups. According to the National Institute of Mental Health (NIMH), major depressive episodes among young adults doubled between 2015 and 2023, with rates climbing from 10.7% to 20.1%. Youth between 12 and 19 now face the highest prevalence of any generation, with suicide attempts—especially among teenage girls—reaching record highs.“What we’re seeing isn’t just a temporary surge—it’s a seismic shift in public mental health that exposes deep cracks in our care infrastructure,” said Dr. Elena Morales, a clinical psychologist and medical advisor to Fox News. “Many individuals have waited years for access to therapy or medication, while crisis care remains overwhelmed.
The gap between need and availability is becoming impossible to ignore.”
Economic Stress, Social Isolation, and the Hidden Triggers
The pandemic reshaped daily life in ways that accelerated mental health deterioration. Remote work, school disruptions, and prolonged social isolation eroded emotional resilience. A 2024 Fox News survey of 3,500 Americans found that 68% reported worsening mental health due to financial instability, job insecurity, or loneliness.Among caregivers, burnout rates now exceed pre-pandemic figures by 35%, according to Census Bureau estimates. Policies aimed at economic recovery have done little to address the toxic ripple effects. “Without stable income, affordable housing, and social connection, treating mental illness becomes a moving target,” stated Dr.
Morales. “Right now, mental health services are treated as optional rather than essential—while hospitals overflow with patients in acute crisis.”
Access in Crisis: Who Can’t Reach Help?
Geographic and socioeconomic disparities compound the challenge. Over 150 million Americans live in federally designated mental health professional shortage areas, with rural regions facing acute provider shortages.Fewer than half of U.S. counties have a single practicing psychiatrist, and wait times for initial appointments often stretch to weeks—if someone can afford private care at $100–$200 per session. Marginalized communities face added barriers.
“Cultural stigma, language gaps, and systemic neglect deepen silence around mental health, especially in communities of color,” noted Dr. Amara Patel, director of behavioral health outreach in underserved urban clinics. “When trusted support is out of reach, desperation normalizes.”
Crisis Care Under Pressure: Breaking Neural Limits
Hospitals and emergency services now ring alarms as daily volumes strain emergency mental health facilities.Psychiatric beds sit at less than 30% capacity nationally, despite a 40% increase in demand since 2020. Suicide attempts are pushing intensive care units to near overflow, delaying life-saving interventions. One Chicago crisis center reported responding to one mind-health crisis every 12 minutes in peak months.
Telehealth showed early promise during lockdowns but now faces new hurdles. Connectivity issues, digital literacy gaps, and privacy concerns limit its reach, particularly among older adults and low-income families. Meanwhile, juvenile mental health facilities struggle to keep pace, with waiting lists stretching into months for children in acute distress.
Public Demand Fuels Policy Push – What’s Being Done?
Federal and state leaders increasingly recognize the urgency. The 2024 Mental Health Access Expansion Act proposes doubling funding for community clinics and telehealth integration, with a goal of delivering 100,000 new mental health slots nationwide by 2027. Several states have launched school-based wellness programs, including mindfulness training and peer support networks—modeled after successful pilot initiatives in California and Maine.Still, progress lags. “Congress has affirmed the need, but funding remains slow and fragmented,” said Dr. Morales.
“We need coordinated, long-term investment—not just short-term fixes—to prevent further deterioration.”
Community Voices: Stories Behind the Numbers
For many impacted, statistics mean little without human context. Among them is Maria Gonzalez, a single mother of three in Houston, who waited 18 months for counseling after her husband’s overdose triggered her depression.


Related Post

Dee Der Blanchard Crime Scene Photos: A Chilling Glimpse Into a Tragic American Case

Korku Filmleri’s Turkish-Dubbed Film Selections (2016): Redefining Audio Accessibility in Turkish Cinema

Revolutionize Web Interactions: How Gs Ajax Powers the Next Generation of Dynamic User Experiences

Colorado Time Rn: The State’s Unique Rhythm Shapes Life, Work, and Wellbeing

