Can You Really Control What You Say After Wisdom Teeth Removal?
Can You Really Control What You Say After Wisdom Teeth Removal?
High tooth extraction often brings unexpected challenges—pain, swelling, and medical advice—but one curious question lingers: Can patients truly control their speech patterns post-surgery? While the physical effects of wisdom teeth removal are temporary and often manageable, the subtle shifts in jaw function, sensory sensitivity, and recovery process influence how individuals communicate—sometimes without realizing it. This article explores the nuanced reality of postoperative speech adjustment, revealing how—and when—control is possible, even after oral surgery.
After wisdom teeth extraction, especially through surgical removal, the body enters a healing phase that directly impacts jaw movement and muscle function. The surgery, though minimally invasive in many cases, temporarily alters neuromuscular coordination. “The surgical trauma—cutting gums, exposing bone, and disrupting soft tissue—means the jaw must heal gradually,” explains Dr.
Elena Torres, oral surgeon at Metro Oral Health. “This temporary stiffness or reduced jaw mobility subtly affects articulation and vocal tone.” Patients often notice these physical changes manifesting in speech. Words may feel mismanaged—voice quality can shift, pronunciation sharper or muddled, and pace altered.
For instance, articulatory precision suffers when the tongue or jaw stabilize in limited motion. “Simple sounds like ‘s,’ ‘t,’ and ‘th’ rely on precise tongue-jaw interaction,” notes speech pathologist Dr. James Holloway.
“If jaw movement is restricted, even by a few millimeters, clarity suffers.” Yet, while physical restrictions set boundaries, they do not dictate complete loss of control. Controlled speech after extraction hinges on patient awareness and adaptive effort. The key lies in recognizing when and how jaw function shifts, then consciously adjusting behavior.
Key strategies include: - **Pacing speech output** - **Modulating volume and articulation** - **Using visual cues to maintain clarity** - Engaging in gentle jaw mobility exercises recommended by clinicians “Many patients surprise us with their ability to adapt,” says Dr. Torres. “By slowing speech tempo and focusing on clear consonant production, they regain balance faster—even days after surgery.” Certain behaviors prove essential to maintaining effective communication.
Speaking too quickly amplifies mispronunciations when jaw motion is limited. Instead, patients benefit from pausing intentionally between phrases, giving themselves time to coordinate movements. Articulation of fricatives and plosives improves through deliberate practice—over-enunciating ‘s’ and ‘k’ when swallowing or opening the mouth minimizes confusion.
Sensory changes following extraction further influence speech. Oral tissues are highly innervated; post-op numbness or tingling alters proprioception—the body’s awareness of its positions. This sensory disruption can delay reaction times in speech, making real-time correction difficult.
“Patients must be patient,” warns speech pathologist Holloway. “The nervous system needs healing before it fully trusts joint feedback again.” Practical exercises shorten recovery time and boost control. For example: - Repeating tongue twisters like “She sells seashells” daily during recovery strengthens motor memory.
- Recording voice samples helps track progress and identify problematic sounds. - Drinking room-temperature water slowly enhances swallowing coordination, supporting clearer pronunciation. Importantly, while temporary speech changes are routine, persistent difficulty warranting medical review is rare.
If slurred speech, drooling, or severe sound distortion continues beyond the expected healing period—usually 1 to 3 weeks—referral to an oral surgeon or speech therapist may be necessary to rule out complications like dry socket, infection, or nerve involvement. Lifestyle choices also shape the clarity of post-surgical speech. Smoking and carbonated drinks irritate healing tissues, increasing swelling and discomfort—factors that indirectly impair speech control.
Staying hydrated, avoiding spicy or acidic foods, and maintaining gentle oral hygiene reduce healing obstacles. Limiting voice strain—no shouting or prolonged speaking—gives tissues space to recover fully, supporting smoother speech patterns over time. Organizations such as the American Association of Oral and Maxillofacial Surgeons emphasize patient education as a cornerstone of recovery.
“Empowering patients with realistic expectations about temporary speech changes leads to greater confidence,” notes Dr. Torres. “Understanding that altered clarity is normal—and actionable—greatly reduces anxiety and improves postoperative communication.” From the clinic to daily life, managing speech after wisdom teeth removal reveals the body’s resilience and the mind’s adaptability.
While surgery imposes physical limits, conscious communication strategies restore control piece by piece. Most patients learn to navigate the postoperative period with surprising ease—adjusting pace, refining articulation, and leveraging simple tools to regain clarity. This blend of biology, behavior, and awareness proves that while surgery changes the mouth, it does not silence the voice.
Ultimately, controlling what you say after wisdom teeth removal is less about willpower and more about informed adaptability. With patience, targeted practice, and professional guidance when needed, patients regain not just physical healing, but linguistic confidence—proving that even in the face of oral surgery, the power to communicate remains within reach.




Related Post

Chiropractic Innovation Meets Ancient Principles at Mondragon Chiropractic
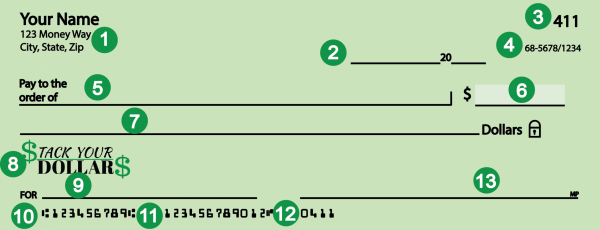
Decode Every Detail: What You Must Know About Navy Federal Routing Numbers
Is Oracle VirtualBox Truly Secure? A Deep Dive into Risks, Safeguards, and Best Practices

Love In Huntsville: Where Romance Blooms Amid Heritage, Nature, and Community

